Szeghalom bőrgyógyászat magánrendelés
csopak időkép
Dr
jófogás ingyen elvihető budapest
. Pancratz Helga Bőrgyógyász, Szeghalom - WEBBeteg. Dr. Pancratz Helga Bőrgyógyász Cím: Békés | 5520 Szeghalom, Dózsa György út 34. magánrendelés 66/371-645 [email protected] Specializáció: Kozmetológus;Klasszikus bőrgyógyászat, gyermek bőrgyógyászat, kozmetológia Rendelési idő: H, Sze: 15-17 Csak előzetes bejelentkezés és időpont egyeztetés után! További Bőrgyógyász orvosok VISSZA A KERESÉSHEZ. Szeghalmi Rendelőintézet – Békés Megyei Központi Kórház. A Békés Megyei Központi Kórház szeghalmi Rendelőintézete 1974-ben kezdte meg működését a Szeghalom, Ady Endre utca 1/b. szám alatt, ahol 2008. óta felújított környezetben 12 szakrendelésen és 3 gondozóban fogadjuk pácienseinket. A Rendelőintézet a 06-66/371-796-es, 06-66/473-590-es és a 06-66/473-589-es telefonszámokon .. Egészségügy - Szeghalom Város Honlapja
hatalom gyűrűi 4 rész
. ORVOSOK Háziorvosok Gyermekorvosok Fogorvosok VÉDŐNŐI SZOLGÁLAT Védőnők ORVOSI ÜGYELET Az orvosi ügyeletet az alábbi telefonszámokon lehet hívni: 06-70/37 03-104 Rendelési idő Pándy Kálmán Kórház Pándy Kálmán Kórház Fekvő- és Járóbeteg Egysége Cím: Szabolcs vezér u
minimálbér 25 év alatt
. 9. Telefon: 371-222, 473-902 Pándy Kálmán Kórház, Vezető főorvos telefon: 473-903
az én környékemen
. Orvosaink - evadoma.hu. Évadoma Magán Egészségügyi Szolgálat. Cím: 5520 Szeghalom Szabadság tér 10-12. fsz. 13. Telefon: +36 20 212 5627. Email cím: [email protected]. Bőrgyógyászat - Medicover. Bőrgyógyászati vizsgálat menete. A vizsgálat a beteg kórelőzményének (anamnézisének) felvételével kezdődik. A bőrgyógyász részletesen kikérdezi a pácienst a tüneteiről, korábbi betegségeiről, esetleg a családban előfordult betegségekről. Ezt követően a bőrgyógyász megvizsgálja az elváltozott bőrfelületet.. Dr. Varga Anita – bőrgyógyász és klinikai onkológus szakorvos. Magánrendeléseim: – Szeged, Kállay Albert u. 7. (Proaktív Egészségközpont) – Baja, Madách Imre u. 6. Időpontfoglalásért kérem hívja a +36 70 259 1687-es telefonszámot. Dr. Varga Anita Bőrgyógyász és klinikai onkológus Osztályvezető klinikai szakorvos Szegedi Tudományegyetem Fontos a rendszeres bőrrákszűrés. Dr. Kun Andrea Bőrgyógyász - Szolnok. Dr. Kun Andrea Bőrgyógyász. Dr. Kun Andrea bőrgyógyász-kozmetológus vagyok, szolnoki bőrgyógyászati magánrendelőmben várom kedves pácienseimet. email: [email protected]. telefon: +36 70 231 7307 cím: 5000 Szolnok, Madách u. 1. Dr. Kun Andrea Bőrgyógyász. Ön is szeretne saját eCardot? Kérem az eCardomat!. Dr. Belső Nóra - Bőrgyógyász szakorvos. Üdvözlöm, dr. Belső Nóra egyetemi tanársegéd vagyok, bőrgyógyász szakorvos. 2006 óta dolgozom az SZTE Bőrgyógyászati és Allergológiai klinikán. A járóbeteg (általános-sürgősségi ambulancia) és fekvőbeteg (általános bőrgyógyászat, allergológia és immunológia) ellátásban is részt veszek.. Bemutatkozás. Évadoma Magán Egészségügyi Szolgálat. Cím: 5520 Szeghalom Szabadság tér 10-12. fsz. 13. Telefon: +36 20 212 5627. Email cím: [email protected]
belépés a facebook fiókomba
. evadoma.hu - RENDELÉSEINK. Bőrgyógyászat. A kezelést a betegek aktuális állapotához és igényeihez igyekszünk igazítani, alaposan mérlegelve annak várható eredményeit és .. Szakrendelések – Békés Megyei Központi Kórház">Szakrendelések – Békés Megyei Központi Kórház. A Békés Megyei Központi Kórház Dr. Réthy Pál Tagkórházában 2020. december 21-től az alábbi járóbeteg szakrendelések helye módosul: – a terhesgondozó szakrendelés az A épület földszintjén 009-es helyiségébe (a kórház területén lévő sebészeti tömb) fogadja a kismamákat, akik a pre-triage. után mehetnek a .. Foglaljorvost.hu. Tüdőgondozó Szeghalom (egyéni l. t.) 11.Tüdőgondozó Szeghalom (csoportos lt.) 2. Addiktológiai gondozó Tüdőkórház

számmisztika személyes év 2020
burger king keszthely
. Botos Zoltán osztályvezető főorvos: 3.Belgyógy, 1.Endokrin. dr. Taybani Zoltán osztályvezető főorvos: 4.Belgyógy., 2.Gasztro.. Szeghalom – Békés Megyei Központi Kórház">Szeghalom – Békés Megyei Központi Kórház. Osztályunk Szeghalmon, a Szabolcs vezér u. 9. szám alatt található. 1943-ban nyílt meg tüdőkórházként, majd 1971-ben került sor utókezelő kórházzá való átszervezésére, 1997-től üzemel a Békés Megyei Pándy Kálmán Kórház Krónikus Belgyógyászati Osztályaként.. Madentko Klinika-Szombathely - Magyar Céginfó
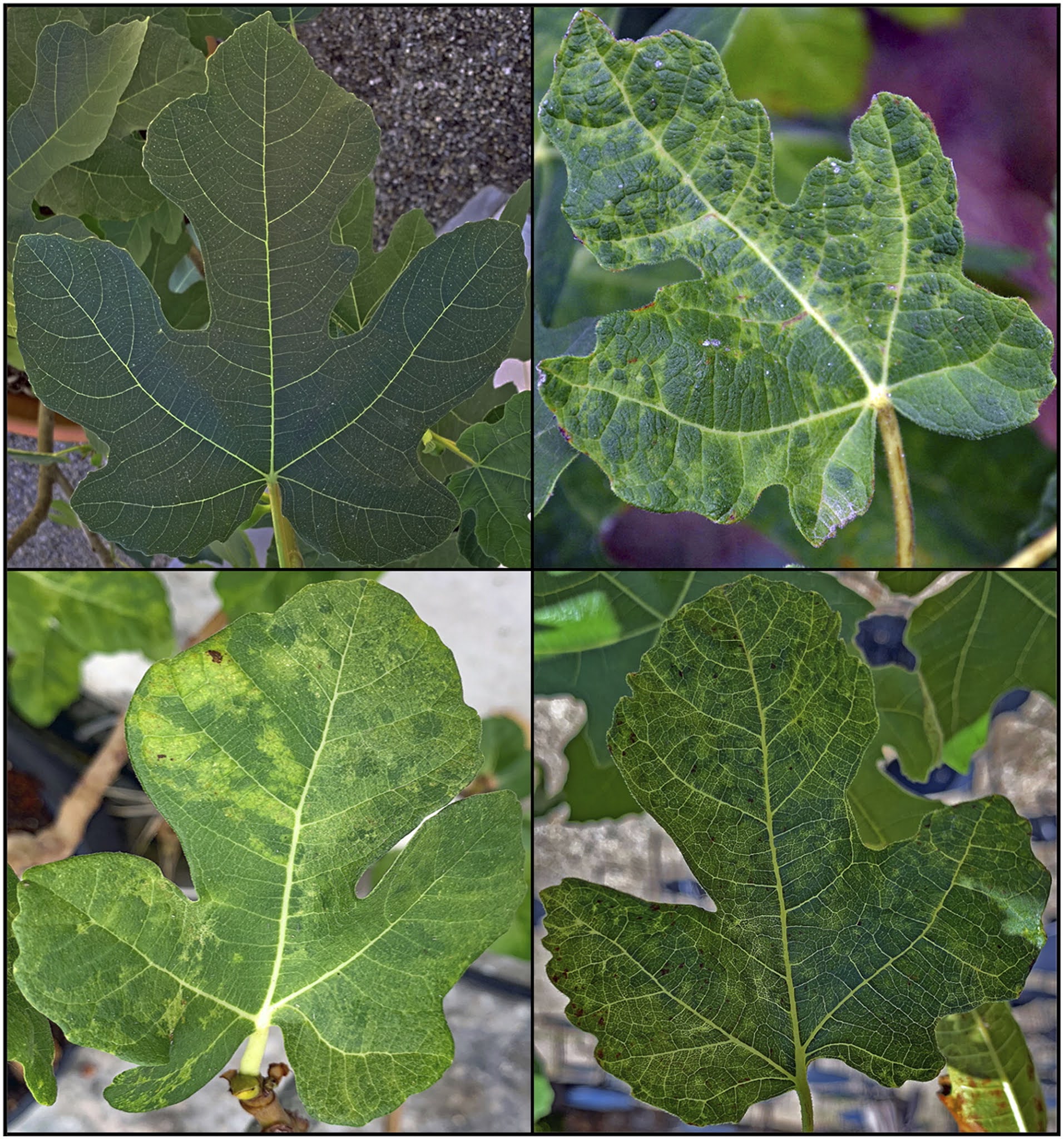
fikusz elastica
. Cím: 9700 Szombathely, Széchenyi u. 4-6
cataflam dolo rapid betegtájékoztató
gül baba krumpli
. (Fő tér - Székesegyház között) Telefon (titkárság): +36 94 318-800 Fax: +36 94 336 500 Porta szolgálat: +36 94 312-047 Dr. Kolbenheyer Ottó vagyok, a cég ügyvezetője és alapítója. Magánklinikánkat 1990-ben alapítottuk és 1994


felnőtt autizmus teszt
. Krónikus bőrbetegségek: urticaria, eczema, psoriasis, pyoderma, vírusos, bakteriális betegségek .. Bőrgyógyászat I.-II.-III. – Békés Megyei Központi Kórház">Bőrgyógyászat I.-II.-III. – Békés Megyei Központi Kórház. III. Bőr- és Nemibeteg Gondozó VI. Bőr- és Nemibeteg Szakrendelés Orvos: Dr. Bérci Zsuzsanna bőr-, nemigyógyász és kozmetológus főorvos Rendelés helye: I

london harry potter múzeum belépő
. Rendelési idők: Kedd, Csütörtök, Péntek: 13.00 .. Bőrgyógyászat Budapest - Móricz Medical Center">Magán Bőrgyógyászat Budapest - Móricz Medical Center. Bőrgyógyászat magánrendelés árak. Bõrgyógyászati szakorvosi vizsgálat 42. 000 Ft. Bõrgyógyászati szakorvosi kontrollvizsgálat 32. 000 Ft. Hétvégi díj kiegészítő *+ 8.000 Ft. Krónikus bőrbetegségek: urticaria, eczema, psoriasis, pyoderma, vírusos, bakteriális betegségek vizsgálata és kezelése 42. 000 Ft..